Report Highlights How States Can Help People Leaving Prison and Jail Get Mental Health Care and Substance Use Treatment
The National Reentry Resource Center released Critical Connections, a discussion paper that identifies key questions state and local leaders should ask as part of their efforts to help people leaving prison and jail with mental health needs get community-based treatment.
“In my state of Michigan, and indeed every state, connecting people leaving prison or jail with mental health or substance use treatment often depends on their access to health care coverage—with public health care coverage, such as Medicaid, playing a particularly vital role,” said Lynda Zeller, deputy director of Behavioral Health and Developmental Disabilities for Michigan’s Department of Health and Human Services.
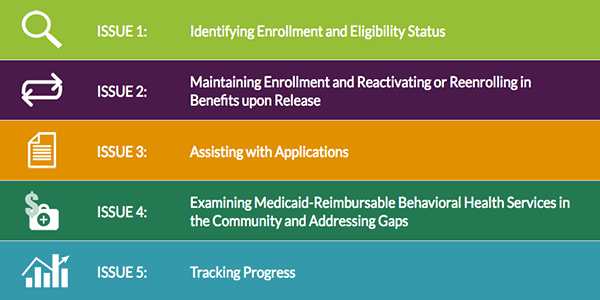
While eligibility for publicly funded health care coverage and the type of treatment and services that coverage supports varies from state to state, government officials in every jurisdiction must work through a common set of challenges to connect eligible people leaving prison and jail to mental health care and substance use treatment. In an effort to address many of these challenges corrections and state and local policymakers face, Critical Connections focuses on five key issues:
Within each of these issues, Critical Connections poses questions that state and local officials should consider when looking to facilitate access to treatment and services in the community. Drawing on examples from local practices and state legislative and administrative actions in 30 states, the paper illustrates how leaders in different states have worked through these considerations using a wide range of strategies.
For instance, while every state must consider how it assists people who are scheduled to be released from prison or jail to apply for health care coverage, the paper examines the varying ways states provide assistance with the applications and when and how this assistance is provided (Issue 3). Examples of how states have addressed these matters include Ohio, where peer educators working inside the prison ensure that people are enrolled, connected to managed care plans, and have a transition plan in place prior to release—and Oklahoma, where the Department of Corrections has a memorandum of understanding in place with the Social Security Administration to streamline access to Supplemental Security Income (SSI) and Social Security Disability Insurance (SSDI) benefits prior to release, particularly for people with mental illnesses.
“In developing this paper, the CSG Justice Center and its partners recognize that state and federal health care policies are in constant flux and will continue to shift, possibly dramatically, in the coming years,” said Tracy Plouck, director of the Ohio Department of Mental Health and Addiction Services.
John Wetzel, director of Pennsylvania’s Department of Corrections, added, “Regardless of where you stand on Medicaid, the Affordable Care Act or any other government-funded health care and benefits, the issues remain the same: A large number of people need behavioral health care coverage and quality treatment and services to help them avoid cycling through prison or jail. So, this paper will be an indispensable resource to policymakers seeking to reduce recidivism and promote recovery.”
Critical Connections was made possible through funding and support from the U.S. Department of Justice’s Bureau of Justice Assistance. The paper examines the varying approaches states have taken to connect eligible people who are released from prison and jail to the mental health care and substance use treatment they need by ensuring health care coverage through some combination of Medicaid, SSI/SSDI, and veterans’ benefits.
“We recognize there is no one-size-fits-all approach to an issue as complicated as this one,” said Denise O’Donnell, director of the Bureau of Justice Assistance. “This paper demonstrates just how much innovation is occurring across the nation, and in doing so, highlights opportunities for state and local leaders to learn from each other.”
********This application deadline has passed******** With support from the U.S. Department of Justice’s Office of…
Read MoreUnlike drug courts, which have been informed by national standards for 10 years, mental health courts (MHCs)…
Read More Building a Better Mental Health Court: New Hampshire Judicial Branch Establishes State Guidelines
Read More
Building a Better Mental Health Court: New Hampshire Judicial Branch Establishes State Guidelines
Read More
 Apply Now to Join a Community of Practice on Police-Mental Health Collaboration Staff Wellness
Apply Now to Join a Community of Practice on Police-Mental Health Collaboration Staff Wellness
With support from the U.S. Department of Justice’s Office of Justice Programs’…
Read More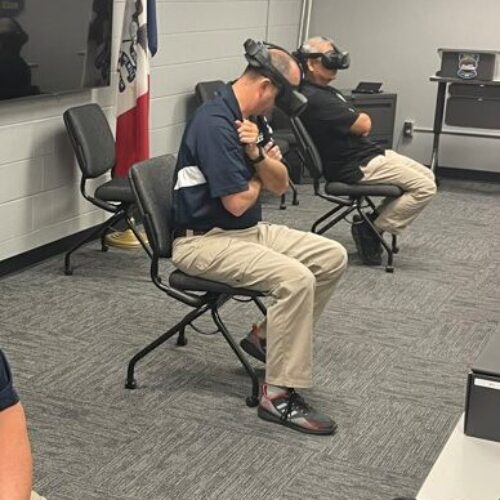 Empathetic Policing: Mason City Police Department Launches Virtual Reality Training Program to Help Officers Better Understand Behavioral Health Crises
Read More
Empathetic Policing: Mason City Police Department Launches Virtual Reality Training Program to Help Officers Better Understand Behavioral Health Crises
Read More
 Biden Signs Six-Bill Spending Package Funding Key Criminal Justice Programs
Biden Signs Six-Bill Spending Package Funding Key Criminal Justice Programs
On March 9, 2024, President Joe Biden signed a $460 billion spending…
Read More