Parity in Mental Health and Substance Use Coverage Will Expand Access to Care
For the millions of individuals involved in the criminal justice system who have mental health or substance use disorders, research suggests that evidence-based treatment can improve health outcomes and reduce future offenses. The rate of mental illness among inmates is at least three times higher than in the general population. Yet, fewer than half report ever receiving mental health treatment. Similarly, the majority of all jail and prison inmates meet criteria for having a substance use disorder, but only a small percentage of these individuals receive treatment services, especially upon reentry to the community. According to the National Institute on Drug Abuse (NIDA), less than 18 percent of individuals who are incarcerated receive substance use disorder treatment either during or following incarceration.
One factor that has long limited access to appropriate treatment services is the lack of health care coverage for all types of behavioral health services. Recently, however, the U.S. Department of Health and Human Services (HHS) took an important step toward addressing this gap. On November 13, 2013, HHS released final rules implementing the Mental Health Parity and Addiction Equity Act (MHPAEA). Under MHPAEA—a federal law passed with bipartisan support in 2008—large, private group health insurance plans offering benefits for mental health and substance use disorders must manage benefits in a manner that is no more restrictive than medical/surgical benefits are managed.
The final rules outline what this means in practice. For instance, insurance plans cannot charge a separate deductible for mental health and substance use disorder services; there must be a single deductible for all services. Insurance plans also cannot charge higher copays for mental health or substance use disorder services or impose a more restrictive limit on the number of behavioral health care visits than they do for medical/surgical visits. The final rules address a host of other issues to ensure equitable treatment of medical/surgical and behavioral health benefits, including network adequacy, provider qualification standards, medical necessity determinations, formulary design, step-down therapy requirements, and exclusions on coverage of court-ordered holds.
If the MHPAEA protections applied only to private group health plans, the potential impact on individuals involved with the criminal justice system would be limited in scope. However, prior laws extended these protections to the Children’s Health Insurance Program (CHIP) and Medicaid managed care plans, and provisions in the Affordable Care Act (ACA) extended MHPAEA protections to individual and small group plans in the private market and to Medicaid plans for the newly eligible.* When combined with the expansion in coverage under the ACA that takes effect in 2014, these expansions of the parity protections mean that the majority of individuals involved with the criminal justice system are soon likely to be eligible for health insurance that is subject to the MHPAEA protections.
This presents an opportunity to improve health outcomes as well as to decrease rates of recidivism. Simply enrolling individuals in a health insurance plan has been found to be associated with a reduction in an individual’s risk of death by as much as 30 percent. On the public safety front, NIDA has estimated that for every $1 spent on addiction treatment, a $4-$7 reduction in the cost of drug-related crime can be expected. Similarly, other studies have shown that improved access to treatment results in lower rates or recidivism and more days in the community. In addition, substantial savings to the corrections system could be achieved by diverting more individuals who do not pose a public safety risk from incarceration to mandated treatment programs.
But to fully realize these potential public health and public safety gains, more work lies ahead. The criminal justice system and its stakeholders can play a key role by helping to enroll the millions of individuals involved with the criminal justice system who are newly eligible for coverage. They can help to monitor and enforce the parity protections and ensure that benefit plans are aligned with and meet the needs of this population. Finally, they can assist in effectively connecting this at-risk population to treatment providers. Doing so will help to realize the opportunities to improve both public health and public safety that are presented by this unprecedented expansion in the availability of comprehensive health coverage for people involved with the criminal justice system who have mental health and substance use disorders
* While the final rules released last month pertain to private coverage, the U.S. Department of Health and Human Services has previously issued guidance on applying parity protections to Medicaid and CHIP, and more guidance is expected in the future.
 This Giving Tuesday, Help Us Break the Cycle of Incarceration, Uphold Justice, and Offer Second Chances
Read More
This Giving Tuesday, Help Us Break the Cycle of Incarceration, Uphold Justice, and Offer Second Chances
Read More
 Vermont Executive Working Group Hears Recommendations on How to Improve Domestic Violence Responses
Read More
Vermont Executive Working Group Hears Recommendations on How to Improve Domestic Violence Responses
Read More
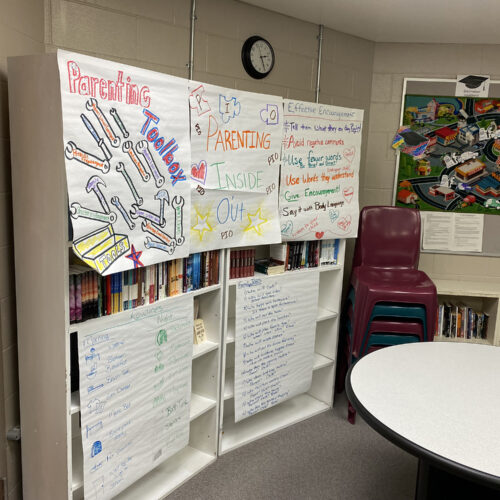 Minnesota Department of Health Leads Cross-County Collaboration to Support Families Impacted by Incarceration
Minnesota Department of Health Leads Cross-County Collaboration to Support Families Impacted by Incarceration
s one of the first points of contact in the criminal justice…
Read More